The field of spinal surgery has seen a significant evolution with the refinement of minimally invasive methods. These procedures offer a distinct alternative to traditional open surgeries, which often involve large incisions and considerable muscle displacement. The core objective of minimally invasive spinal fixation is to achieve stability and fusion while preserving the patient’s native anatomy as much as possible. This approach relies on specialized technology and precise execution to place a spinal fixation system through smaller access points, leading to a cascade of potential benefits for patient recovery.
Core Principles and Surgical Advantages
The methodology behind these techniques centers on precision and minimal tissue disruption. Instead of a long, open incision, surgeons utilize a series of small portals. Through these, they insert specialized dilators and retractors to create a working channel down to the spine, avoiding cutting through major muscle groups. This direct approach allows for the accurate placement of a pedicle screw-based spinal fixation system with far less collateral damage. The primary advantages for the patient are substantial, including reduced intraoperative blood loss, lower risk of infection, and significantly less postoperative pain compared to conventional procedures.
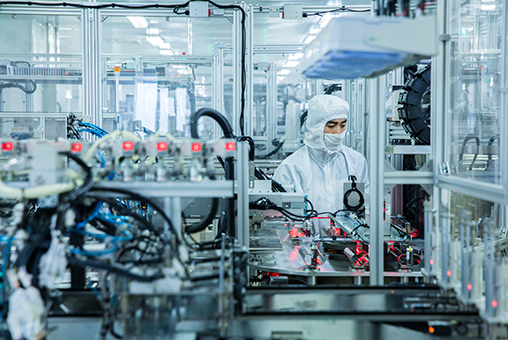
Instrumentation and Procedural Execution
The success of these methods is heavily dependent on specialized instrumentation designed for navigation through confined spaces. A modern spinal fixation system for minimally invasive surgery often includes low-profile screws and rods that can be inserted percutaneously. Surgeons frequently employ real-time imaging guidance, such as fluoroscopy or surgical navigation systems, to visualize anatomy and guide the precise placement of hardware. This enhanced visualization is critical for ensuring screws are positioned correctly within the vertebral pedicles, maximizing the construct’s stability and minimizing the risk of neurological compromise.
Patient-Centric Outcomes and Recovery
The collective impact of these techniques manifests most clearly in the patient recovery trajectory. With less soft tissue trauma, the body’s inflammatory response is markedly reduced. This often translates to shorter hospital stays and a decreased reliance on opioid pain medications during the initial recovery phase. Patients can typically begin mobilization and physical therapy sooner, which is a key factor in returning to daily activities and improving long-term functional outcomes. The goal is not only to address the spinal pathology effectively but to do so in a way that optimizes the entire healing process.
The adoption of minimally invasive techniques reflects a broader commitment to improving surgical care through innovation that prioritizes patient well-being. These procedures demonstrate how technological advancements in instrumentation and imaging can directly enhance clinical results. At WEGO Medical, we support this progress by developing and supplying sophisticated medical devices, including our spinal fixation system, designed to meet the exacting demands of modern surgical protocols. Our role is to provide surgeons with the reliable tools needed to perform these complex procedures with confidence.